胎儿肾脏集合部分离的超声诊断及动态随访
王砺聪a,周凤英b
北京市朝阳区妇幼保健院 a.医务科;b.超声科,北京 100022
[摘 要]目的 探讨超声诊断胎儿肾盂分离的临床意义及产前肾盂宽度的变化趋势。方法 回顾性分析中期妊娠行超声筛查的13500例孕妇中检出胎儿肾盂前后径宽度(Renal Pelvis Anteroposterior Diameter,RPAPD)≥4 mm且无其他畸形的114例胎儿超声资料。结果 胎儿的RPAPD的大小与孕妇年龄之间无明显差异(P=0.062)>0.05;中期妊娠胎儿单侧RPAPD72例(63.15%)多于胎儿双侧RPAPD42例(36.84%);分娩前胎儿单侧RPAPD<10mm的有69例(66.35%)多于胎儿双侧RPAPD35例(33.65%);胎儿肾盂持续性进行性分离≥10 mm单侧3例(30%)少于双侧7(70%);分娩前RPAPD<10 mm与持续性进行性RPAPD≥10 mm组间进行分类变量的卡方检验,P=0.0023<0.05,具有统计学意义。结论 中期妊娠超声诊断单纯胎儿RPAPD(4~10 mm)的患者大部分在分娩前RPAPD<10 mm,RPAPD≥10 mm的患者在分娩前持续性扩张。超声跟踪监测胎儿RPAPD,能及时准确提供产前信息。
[关键词]超声检查;产前检查;胎儿;肾盂分离;肾盂前后径宽度
胎儿肾盂分离是产科超声常见的胎儿泌尿系统异常,文献报道发生率为0.8%~5.5%[1]。超声检查是用于筛查胎儿泌尿系统异常最常用的方法。胎儿肾盂分离的原因不清楚,目前认为主要由于输尿管的功能性阻塞或狭窄,少数是病理性因素,包括肾盂输尿管连接处的阻塞、先天性巨输尿管、多囊肾、重复输尿管及后尿道瓣膜[2]。
1 资料与方法
1.1 一般资料
回顾性分析2012年4月~2015年12月在我院建档并进行产前超声检查的13500例孕妇,年龄20~45岁,夫妇双方均无遗传病史,非近亲结婚。产前20~24周超声共检出胎儿肾集合系统分离≥4 mm的126例,其中伴发其它异常的12例。
1.2 方法
使用Voluson E8或E10及Hitachi Ascendus彩色超声诊断仪,探头频率3~5 MHz。所有胎儿肾脏留取横切面、矢状切面及肾脏血流图,仔细观察双肾大小、位置、有无占位、集合部、皮髓质情况、输尿管有无扩张等,均进行详细记录。采用Toiviainen-Salo等[3]提出的胎儿肾积水诊断标准:孕33周以前肾集合系统前后分离值≥4 mm,孕33周后≥7 mm。同时注意肾盏有无扩张、实质有无变薄等。首次发现肾集合系统分离后,于产前4~6周复查,产后3d复查。
2 统计学分析
应用SPSS 15.0统计软件进行分析,计量资料以平均值±标准差( ±s)表示,分类变量比较采取χ2检验。以P<0.05为差异有统计学意义。
±s)表示,分类变量比较采取χ2检验。以P<0.05为差异有统计学意义。
3 结果
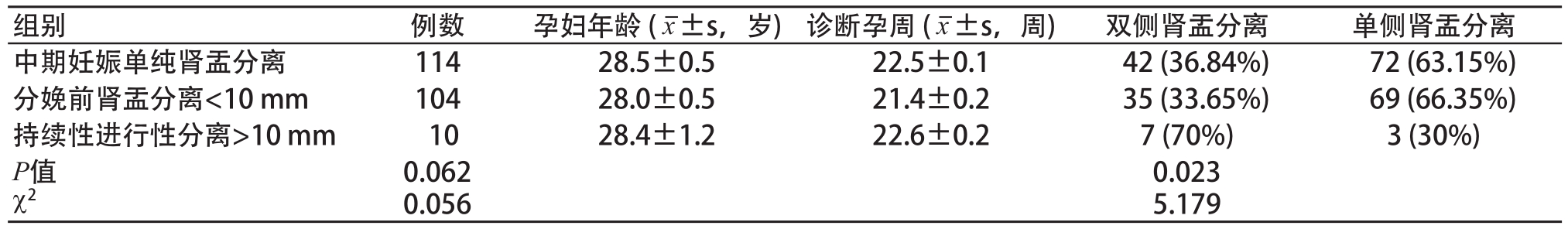
孕妇年龄之间进行t检验,P=0.062>0.05,各孕周之间进行t检验,P=0.056>0.05,差异无统计学意义。胎儿的肾盂分离前后径(Renal Pelvis Anteroposterior Diameter,RPAPD)的大小与孕妇年龄之间无明显差异(P=0.062)>0.05。中期妊娠胎儿单侧RPAPD72例(63.15%)大于胎儿双侧RPAPD42例(36.84%),分娩前胎儿单侧RPAPD<10 mm的69例(66.35%)多于胎儿双侧RPAPD35例(33.65%)。胎儿肾盂持续进行性分离≥10 mm单侧3例(30%)少于双侧7例(70%)。分娩前RPAPD<10 mm与持续进行性RPAPD≥10 mm组间进行分类变量的χ2检验,P=0.0023<0.05,具有统计学意义。具体结果见表1。
中期妊娠超声诊断单纯胎儿RPAPD(4~10 mm)的患者大部分在分娩前RPAPD<10 mm,RPAPD≥10 mm的患者在分娩前持续性扩张。超声跟踪监测胎儿肾盂分离宽度,能及时准确提供产前信息。
4 讨论
超声检查是诊断胎儿泌尿系统异常的首选检查方法,通过对胎儿肾脏的大小、皮髓回声、肾盂分离等详细描述,能发现大多数胎儿肾脏发育异常[4],是产前观察肾脏发育的有效手段。
正常胎儿肾脏孕10周就可产生尿液,在孕17~18周后能常规显示,在膀胱充盈是肾脏集合系统分离最大0.6 cm。孕34周后肾实质厚度趋于稳定,实质厚度在0.5 cm以上[5]。胎儿双肾轻中度集合系统分离大部分能自然恢复正常,为生理性或一过性。胎儿肾集合系统分离原因:孕妇在超声检查前大量饮水,机械性或功能性梗阻导致的一过性梗阻,胎儿泌尿道对孕激素的反应,肾脏血管的压迫,胎儿尿量较多以及胎儿输尿管的顺应性较强、弹性较差等因素有关;少数为病理性,需临床治疗。双肾集合系统分离越大,时间越长,预后越差。
胎儿肾积水是依靠产前超声测量集合系统液性分离前后径的宽度确诊[6]。国内卜凡堂等[7]认为,孕晚期胎儿肾积水<1.63 cm视为可复性;>2.15 cm为不复性,出生后应及时检查及治疗。国外Richard S. Lee等[8]认为妊娠中期0.7~1.0 cm,妊娠晚期0.9~1.5 cm为中度肾积水,妊娠中期≥1.0 cm,妊娠晚期≥1.5 cm为重度肾积水。Toiviainen-Salo等[3]提出的胎儿肾积水诊断标准:孕33周以前肾集合系统前后分离值≥4 mm,孕33周后≥7 mm,对确诊胎儿肾盂积水的灵敏度为100%,但假阳性率为高。孕24周前肾盂分离>4 mm和孕24后肾盂分离>10 mm,灵敏度为80%,假阳性15%。Wollenberg等[9]发现,肾盂分离<10 mm的胎儿生后无泌尿系统感染或手术干预,肾盂分离在10~15 mm的胎儿,生后23%须行泌尿系统的治疗,肾盂分离>15 mm,产后64%治疗。夏春华等[10]报道,在产前诊断的胎儿肾积水中,大部分为肾脏发育过程中机能不够完善而出现的一过性和生理性现象,可随个体发育自行消失。本组资料与国内外专家基本一致。
如果肾盂分离>1.5 cm的即可诊断肾盂积水,一旦明确诊断可以进行干预,对于胎儿肾盂积水严重的,有学者主张提前分娩以尽早采取手术治疗,也有学者主张产前对患儿肾盂或膀胱实施穿刺引流术,术后严密随访[11],目的在于缓解胎儿肾盂积水症状。对于双肾积水胎儿可在宫内进行手术,目前开展较少,且争议大[12]。如果伴发有Prune-Belly综合征、双侧多囊肾疾病及染色体异常,应及时终止妊娠。
表1 各孕期胎儿肾盂分离情况
超声监测产前胎儿肾盂宽度是诊断胎儿肾盂分离最方便、最直接、最准确的检查方法,对于早期区分胎儿病理性肾盂分离,提供准确及时的信息,选择适当的分娩时机,能减轻胎儿父母的焦虑,并且对于儿科医生的术前评估或早期实施干预保护胎儿肾功能[13]也会有所帮助。
[参考文献]
[1] Kim MK,Kim MJ,An JJ,et al.Outcome of isolated fetal renal pyelectasis diagnosed during midtrimester screening ultrasound and cut-off value to predict a persistent or progressive pyelectasis in utero[J].Perinat Med,2013,41(4):401-409.
[2] 朱晨,任芸芸,严英榴,等.超声诊断妊娠中期胎儿单纯肾盂扩张及产前宫内动态随访[J].中华超声影像学杂志,2015,24(8): 697-700.
[3] Toiviainen-Salo S,Garel L,Grignon A,et al.Fetal hydronephrosis: is there hope for consensus?[J].Pediol,2004,34(7):519-529.
[4] 田雨,杨太珠,罗红.产前超声诊断胎儿肾脏发育异常196例临床分析[J].实用妇产科杂志,2012(10):861-864.
[5] 李艳青,周启昌,王小艳,等.胎儿肾积水的产前超声诊断及预后观察[J].长治医学院报,2012,26(1):56-58.
[6] 纪伟英.彩超对胎儿肾积水诊断及预后的综合评价[J].中国超声医学杂志,2007,23(6):457-459.
[7] 卜凡堂,唐淑云,孙丽,等.胎儿肾积水12例超声研究[J].中国超声医学杂志,2001,17(12):934-936.
[8] Richard S,Lee MD,Marc Cendron MD,et al.Antenatal hydronephrosis as a predictor of postnatal outcome: a meta-analysis[J]. Pediatrics,2006,118(2):586-593.
[9] Wollenberg A,Neuhaus T,Willi U,et al.Outcome of fetal pelvic dilatation diagnosed during the third trimester[J].Ultrasound Obst Gyn,2005,25:483-488.
[10] 夏春华,郑艳芬,曾华北,等.彩色多普勒超声诊断及随访胎儿双肾集合系统分离的临床研究[J].中外医学研究,2015,13 (27):42-44.
[11] Soothill PW,Bartha JL,Tizard J.Ultrasound 2 guided laser treatment for fetal bladder outlet obstruction resulting from ureterocele[J].Am J Obstet Gynecol,2003,188:1107-1108.
[12] Quan A.Fetal and neonatal hydronephrosis[J].Early Hum Dev, 2006,82:1-2.
[13] Signorelli M,Cerric V,Taddei F,et al.Prenatal diagnosis and management of mild fetal pyelectasis: implications for neonatal outcome and follow-up[J].Eur J Obstet Gynecol Reprod Biol,2005, 118(2):154-159.
Ultrasonic Diagnosis and Dynamic Follow-Up in Isolated Fetal Renal Pyelectasis
WANG Li-conga, ZHOU Feng-yingb
a. Department of Medical Affairs; b. Department of Ultrasound, Women and Children' Hospital of Chaoyang District, Beijing 100022, China
Abstract:Objective To assess the clinical significance of isolated fetal renal pyelectasis and its changes in utero. Methods One hundred and fourteen isolated pyelectasis cases with their RPAPD (Renal Pelvis Anteroposterior Diameter) ≥ 4 mm without other fetal anomaly who were screened from 13500 pregnant women by using ultrasound were retrospectively reviewed. Results There was no obvious difference between RPAPD and the age of pregnancy (P=0.062)>0.05; 72 cases (63.15%) were one sided renal pyelectasis, more than 42 cases (36.84%) of renal pyelectasis were on both sides; 69 cases (66.35%) were one sided renal pyelectasis and RPAPD < 10 mm before delivery, more than 35 cases (33.65%) with bilateral renal pyelectasis and RPAPD < 10 mm; 3 cases with RPAPD ≥ 10 mm (30%) and one sided renal pyelectasis were treated with continuous renal pelvis separation, less than 7 cases with RPAPD≥ 10 mm (70%) and bilateral renal pyelectasis; According to the Chi-square test between two groups (RPAPD < 10mm Before Gelivery Group and RPAPD ≥ 10 mm Continuous Renal Pelvis Separation Group), the difference was statistically significant (P=0.0023<0.05). Conclusion Although most of the fetuses with RPAPD ranging from 4 to 10 mm in second trimester would remain the same or resolved before delivery, those with RPAPD ≥ 10 mm might continuously expand. Tracking and monitoring of fetal renal pelvis by using ultrasound could provide proper prenatal consultation.
Key words:ultrasonography; prenatal examination; fetus; renal pelvis separation; renal pelvis anteroposterior diameter
[中图分类号]R445.1;R714.5
[文献标识码]B
doi:10.3969/j.issn.1674-1633.2016.11.014
[文章编号]1674-1633(2016)11-0059-03
收稿日期:2016-02-18
通讯作者:周凤英,主任医师,研究方向:妇产科超声。